Human Metapneumovirus (HMPV)
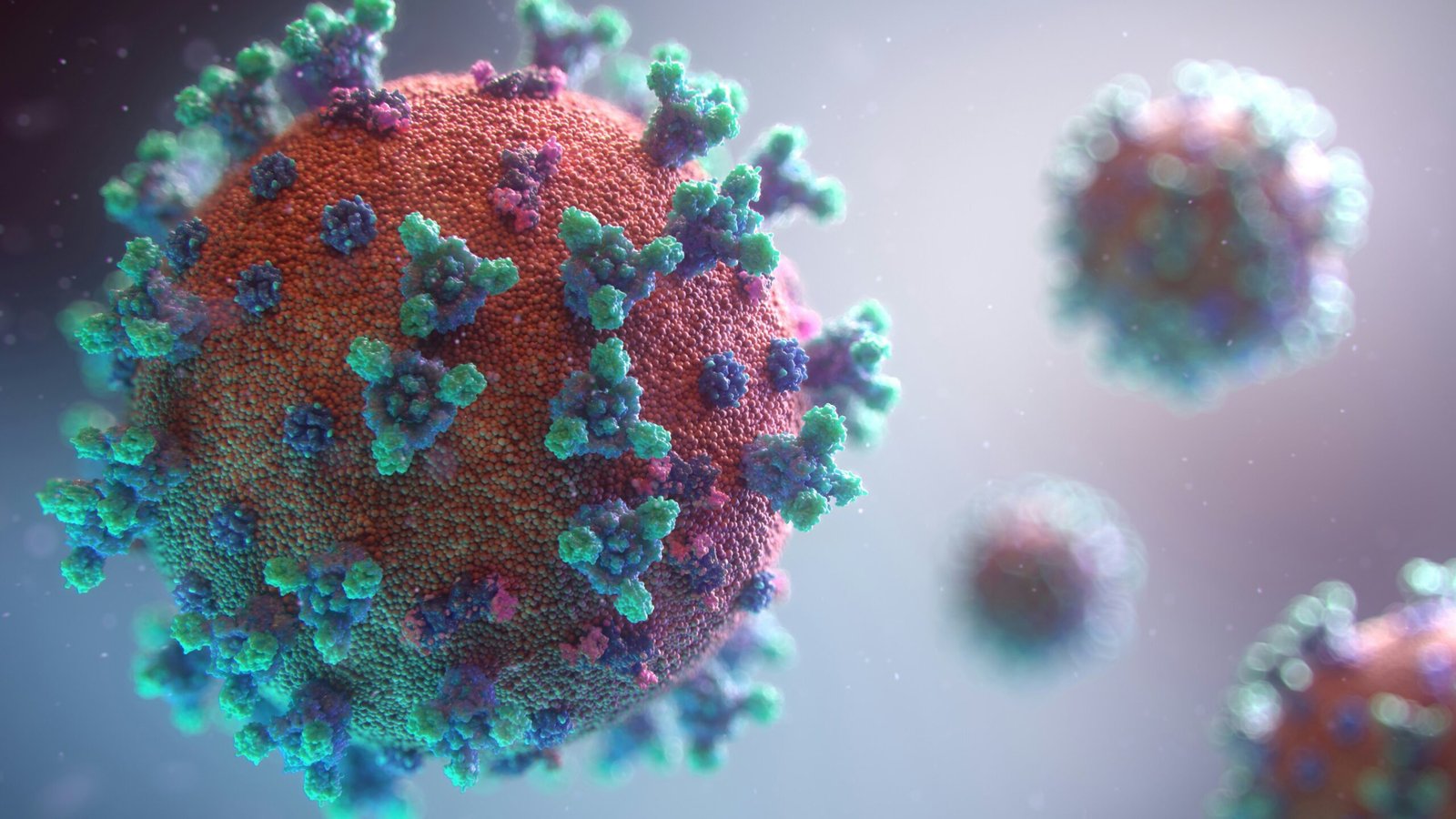
Human metapneumovirus (HMPV) is a member of the Paramyxoviridae family, categorized under the Metapneumovirus genus. This virus was first identified in the year 2001 by a team of researchers in the Netherlands who were studying respiratory infections in children. Since its discovery, HMPV has been recognized as a significant pathogen contributing to respiratory illnesses worldwide, particularly in children and the elderly, although it can affect individuals of any age.
Biologically, HMPV is an enveloped, single-stranded RNA virus that targets the respiratory epithelium. Upon entering the host’s respiratory tract, it attaches to the cellular receptors on the surface of respiratory cells, facilitating its entry. Once inside the cell, HMPV hijacks the host’s cellular machinery to replicate itself, leading to the production of new viral particles. This replication process can result in cellular damage, inflammation, and the manifestation of respiratory symptoms akin to other viral infections such as influenza and respiratory syncytial virus (RSV).
The clinical presentation of HMPV infection can range from mild to severe, with symptoms often resembling those of other common respiratory viruses. These symptoms may include cough, wheezing, and difficulty in breathing, particularly in vulnerable populations, which underscores HMPV’s relevance in public health discussions. Although it has similarities with other viral pathogens, distinct epidemiological patterns have emerged, revealing the unique burden of HMPV. The virus circulates primarily in the late winter and spring months, leading to seasonal outbreaks that can significantly impact healthcare systems.
Prevalence of HMPV Cases in China
Human Metapneumovirus (HMPV) is increasingly recognized as a significant viral pathogen affecting respiratory health across various populations, including in China. Recent studies reflect a growing incidence of HMPV cases, particularly during the winter months when respiratory illnesses tend to surge. The prevalence rates vary annually, with some reports indicating that approximately 5% to 10% of respiratory infections in children and adults are attributed to HMPV, marking a notable trend in viral respiratory infections in the region.
Statistical data reveal fluctuations in HMPV cases, often correlated with broader epidemiological trends. For instance, the annual surveillance data from major healthcare institutions in China denote rising HMPV infections from 2018 to 2022, suggesting an increasing impact on public health. Furthermore, studies have reported an uptick in HMPV cases during outbreaks of other respiratory viruses such as influenza and SARS-CoV2, implying potential interactions between these viruses and the impact of concurrent infections on overall severity.
A multifaceted approach is necessary to understand the increasing prevalence of HMPV cases. Environmental factors, such as climate variations and air quality, contribute significantly to viral transmission. Additionally, social determinants, including population density and healthcare access, play a critical role in the risk of infection. In urban settings, high levels of pollution and increased contact among individuals may further exacerbate the spread of HMPV. Moreover, China’s healthcare system faces challenges in timely diagnosis and proper reporting, which can hinder accurate data collection and understanding of the virus’s impact. By examining these various elements, health authorities can better address the complexities surrounding HMPV cases and implement more effective interventions moving forward.
Symptoms of HMPV Infection
Human metapneumovirus (HMPV) infections manifest with a variety of symptoms that can vary significantly among different age groups and populations at risk. The symptoms typically appear 3 to 6 days following exposure to the virus, and they can range from mild to severe. Common symptoms associated with HMPV infections include fever, cough, runny or stuffy nose, and sore throat, which resemble those seen in other viral respiratory illnesses. These symptoms often lead to a similar clinical presentation, making it challenging to distinguish HMPV from other respiratory viruses such as influenza or respiratory syncytial virus (RSV).
In children, especially infants, HMPV can lead to more severe respiratory issues, including wheezing, difficulty breathing, and even bronchiolitis or pneumonia in young children and those with underlying health conditions. The incidence of HMPV is particularly concerning in this demographic, as it can result in hospitalizations during peak seasons of respiratory infections. Adults, particularly those with weakened immune systems or chronic respiratory diseases, may also experience pronounced symptoms and complications due to HMPV.
Less common symptoms may include gastrointestinal upset and fatigue, although these are not as widely reported. There may also be differences in symptomology based on individual health status and age, where those with existing health complications may experience a more protracted illness. This variability in symptoms underscores the importance of clinical recognition and timely management of HMPV cases. Overall, while HMPV infections predominantly present with respiratory symptoms similar to other viral illnesses, their unique patterns and presentations can be critical for accurate identification and treatment. Awareness of these symptoms is essential in mitigating the impact of HMPV and ensuring that at-risk populations receive appropriate care.
Comparative Analysis of HMPV and Other Respiratory Viruses
Human Metapneumovirus (HMPV) is one of several viruses that contribute to respiratory illnesses, with influenza virus and respiratory syncytial virus (RSV) being other notable contenders. Understanding the similarities and differences between these pathogens is crucial for effective public health strategies.
Transmission of HMPV is similar to that of influenza and RSV. All three viruses can spread via respiratory droplets when an infected person coughs or sneezes. They can also survive on surfaces, posing additional risk for indirect transmission. However, HMPV generally exhibits a lower rate of transmission compared to influenza, which is notorious for its rapid spread during peak seasons.
In terms of symptoms, HMPV typically presents with mild to moderate respiratory issues, such as cough, fever, and wheezing, akin to those caused by RSV. However, unlike RSV and influenza, HMPV often leads to milder symptoms in adults and older children. Infants and individuals with weakened immune systems are at higher risk for severe manifestations, paralleling the demographics most susceptible to RSV.
Regarding the severity of illness, HMPV can lead to hospitalization, especially in vulnerable populations, albeit less frequently than severe influenza cases. Influenza is known for its dramatic seasonal spikes in hospital admissions, while HMPV cases tend to be more sporadic and less well-documented. Consequently, significant attention is often placed on influenza vaccines, overshadowing the potential impact of HMPV.
In summary, while HMPV shares many characteristics with other respiratory viruses such as influenza and RSV, its unique transmission patterns, symptom severity, and affected demographics warrant specific consideration in the broader context of public health. Recognizing these differences may enhance disease management strategies and underscore the importance of comprehensive surveillance of hmpv virus cases and their implications for at-risk populations.
Emerging Trends: New Variants of HMPV
The Human Metapneumovirus (HMPV) has garnered increased attention due to the emergence of new variants in recent years. Researchers continue to investigate the mutations that have occurred within the HMPV genome, which are essential in understanding the virus’s impact on transmissibility and virulence. Current studies indicate that some of these variants may possess enhanced capabilities to evade immune responses, raising concerns about their potential implications for global health.
Notably, ongoing research is focused on the genetic sequencing of these HMPV variants. This genomic analysis enables scientists to identify specific mutation patterns that could affect how the virus interacts with host immune systems. As new variants emerge, it is crucial for public health officials to monitor these changes, as they may alter the risk profile associated with HMPV infections. An understanding of emerging HMPV virus cases is vital for predicting future outbreaks and bolstering community health initiatives.
Additionally, the impact of emerging variants extends beyond just the biology of the virus; it also influences the strategies employed to combat infections. The vaccination landscape for HMPV must adapt to these changes. Researchers are exploring the potential need for updated vaccines that are effective against the variants. The speed at which new variants arise necessitates a flexible approach to vaccine development, ensuring that public health responses remain relevant and effective in controlling the spread of HMPV.
In conclusion, continuous monitoring of HMPV variants is essential for understanding their implications on public health. As research progresses and new variants are identified, it will be crucial to adapt our responses to mitigate the risks associated with HMPV infections. A vigilant, informed approach will aid in managing the potential threat posed by evolving HMPV virus cases in the community.
Impact of HMPV Outbreaks in China
The emergence of Human Metapneumovirus (HMPV) outbreaks in China has presented significant challenges to public health and the healthcare system. As an important respiratory virus, HMPV is primarily known for causing respiratory illnesses, particularly in children and the elderly. Recent outbreaks have raised concerns regarding the transmission dynamics and the strain these cases place on healthcare infrastructure.
HMPV virus cases have been observed to lead to increased hospitalizations, particularly during outbreaks. Medical facilities often face overcrowding as the virus can spread swiftly, especially within vulnerable populations. This has necessitated a re-evaluation of resource allocation, leading to a heightened demand for antiviral medications and supportive care. Health authorities have had to implement triage protocols to manage the influx of patients and ensure that severe cases receive prompt treatment.
The socioeconomic impacts of HMPV outbreaks cannot be overlooked. The strain on healthcare systems translates into increased healthcare costs for families and the government. Furthermore, the fear of infection leads to disruptions in daily activities, affecting economic productivity. Schools and workplaces may see temporary closures, and individuals may experience job losses, particularly in sectors that rely on in-person interactions.
In response to these challenges, Chinese health authorities have conducted extensive public health campaigns aimed at increasing awareness and education about HMPV. Surveillance systems have been enhanced to monitor virus activity, allowing for timely interventions. Vaccination initiatives are being explored, although they remain in developmental phases. Overall, the response to HMPV outbreaks emphasizes the need for a collaborative approach involving public health officials, healthcare providers, and the community to mitigate the impact of such viral infections, ensuring a robust defense against future outbreaks.
Case Studies: HMPV in India and Beyond
Human Metapneumovirus (HMPV) emerges as a significant respiratory pathogen, particularly in pediatric populations. In India, recent studies have shown an increase in HMPV virus cases, especially during the colder months when respiratory infections peak. Data from hospitals indicates that children under five years old exhibit high susceptibility to HMPV, often presenting similar symptoms to those of more prevalent viruses, such as influenza and respiratory syncytial virus (RSV). For instance, a retrospective study conducted in a New Delhi hospital highlighted that around 25% of the pediatric respiratory illness cases were attributed to HMPV, illuminating its role in the respiratory virus profile of the region.
In contrast, examining the experience of China reveals a distinct trajectory in the management of HMPV infections. Since the initial identification of HMPV in 2001, China has seen varying levels of incidence, with significant outbreaks linked to seasonal changes. A comprehensive surveillance program has been established, allowing for better tracking of HMPV cases across urban and rural settings. The Chinese healthcare system’s structured response, including vaccination campaigns and public awareness initiatives, has aided in mitigating outbreaks, underscoring the importance of community health engagement in controlling HMPV transmission.
The comparisons between India’s healthcare response and China’s proactive measures highlight the necessity of tailored strategies for mitigating HMPV virus cases effectively. In India, the challenges often stem from limited access to healthcare facilities in rural areas and variations in disease awareness among communities. Thus, drawing from the Chinese experience can inform India’s approach, emphasizing early diagnosis, efficient reporting of HMPV cases, and enhanced laboratory capacities. Ultimately, understanding the distinctive patterns of HMPV infections within these two countries can pave the way for more effective public health interventions globally.
Preventive Measures and Treatment Options
As the incidence of human metapneumovirus (HMPV) cases continues to gain attention globally, it is crucial to implement effective preventive measures and explore available treatment options. Currently, no specific vaccine exists for HMPV, but research is underway to develop one. Public health initiatives play a significant role in raising awareness about the importance of hygiene and vaccination against other respiratory illnesses, contributing indirectly to the management of HMPV infections.
Read more: Exploring the Development and Impact of Russia’s Cancer Vaccine
Preventive strategies primarily focus on reducing the spread of the virus. Individuals are encouraged to practice standard hygiene measures such as regular handwashing, especially during the peak respiratory virus season. In crowded or healthcare settings, wearing masks can further decrease the risk of transmission. Health organizations recommend minimizing close contact with infected individuals to prevent the spread of HMPV cases.
In terms of treatment, the management of HMPV infections is mainly supportive. Healthcare providers typically focus on alleviating symptoms, which often include cough, fever, and difficulty breathing. Patients with mild symptoms can receive symptomatic treatment, such as fever reducers and cough suppressants. Those with more severe respiratory symptoms may require hospitalization, where oxygen therapy and intravenous fluids can be administered. Antibiotics are not effective against viral infections; therefore, their use is discouraged unless a secondary bacterial infection occurs.
Monitoring the developments in HMPV-related research is essential. Scientists are studying potential antiviral therapies targeting HMPV, which may become available in the future. Ultimately, preventing the spread of HMPV hinges on public health education and effective symptom management. As awareness increases and research advances, our ability to tackle and control human metapneumovirus cases will certainly improve.
Looking Forward: Future Research and Monitoring of HMPV
The landscape of research surrounding human metapneumovirus (HMPV) continues to evolve, necessitating an emphasis on specific areas to foster a comprehensive understanding of this respiratory pathogen. One critical area of focus is the efficacy of potential vaccines. As global health organizations seek to mitigate viral infections, exploring the effectiveness of vaccine candidates against HMPV is imperative. This research will not only evaluate immediate immune responses but also the durability and breadth of protection against various HMPV strains.
Moreover, it is essential to investigate the long-term effects of HMPV infections. Emerging evidence suggests that respiratory viruses, including HMPV, may have lingering impacts on pulmonary health, potentially predisposing individuals to chronic respiratory conditions. Future studies should aim to elucidate the consequences of HMPV infections on individuals over extended periods, particularly among vulnerable populations such as the elderly and those with pre-existing health conditions.
Molecular research is another pivotal area that warrants attention. Understanding the genomic characteristics of HMPV can shed light on its evolution and transmission dynamics. By examining genetic variations in HMPV, researchers can enhance their comprehension of associated epidemiological trends and potentially forecast outbreaks. This information could prove vital, especially as HMPV cases may increase in coincide with other respiratory viruses like influenza or SARS-CoV-2.
In addition to these specific research avenues, it is increasingly apparent that global surveillance efforts are crucial for monitoring HMPV and other respiratory pathogens. Establishing robust surveillance systems will help gather data on incidence rates, mortality, and emerging strains. By fostering international collaboration among researchers, public health officials can better track HMPV virus cases and ensure timely responses to potential outbreaks, ultimately bolstering global health security.
Read more: farm equipment